Recurrent Pregnancy Loss
Recurrent Pregnancy Loss Program: A 360° Approach
Have you been experiencing repeated miscarriages prior to your 20th week of pregnancy? Are you at an advanced fertility age and have consistently struggled with not being able to get pregnant after multiple attempts?
We offer a comprehensive program that assesses all of the aspects that may be leading to recurrent pregnancy loss or repeated failed pregnancies. We take a detailed medical history that is then reviewed by our multidisciplinary team of experts in a dedicated weekly meeting in which we tailor individualized treatment that is holistic in its approach and offers the best cutting-edge treatment based on the most recent scientific data. Our multidisciplinary team of recurrent pregnancy loss experts, made up of world renowned physicians, nurses, pathologists, geneticists, psychologists, perinatologists and acupuncturists offer a unique program to help individuals suffering from recurrent pregnancy loss and/or recurrent implantation failure that is comprehensive, holistic and individualized with the most recent scientific evidence at its core.
Pregnancy loss is multi-factorial. The physicians at HRC work tirelessly to find an etiology and understand how imperative it is to isolate a cause for the loss when able using an individualized approach. Starting with a detailed medical history is key. In doing so, we believe there is both medical and psychological benefit. We also appreciate the expertise and guidance of our neighboring medical professionals and strongly advocate for the value in a comprehensive approach to care. Through our combined 30 years of experience practicing in the Los Angeles area, the physicians at HRC have each developed close professional relationships with nearby nutritionists, dieticians, acupuncturists, therapists and naturopaths. These select individuals, each in their respective areas, focus their practices on recurrent pregnancy loss and complement our care. We believe this combined approach synergizes to elevate the global outcome with a universal goal-to provide the most cutting edge treatment in the area of recurrent pregnancy loss and implantation failure. Beyond the confines of our medical offices, we encourage each patient to be open to our suggested referrals and recommendations to broaden their vision and incorporate these practitioners into their care.
“Our first overall impression is that HCR is very thorough and organized. HCR stood out to us because of the recurrent pregnancy loss program.”
What the Numbers Say
According to RESOLVE: The National Infertility Association

15-20%
… of pregnancies end in multiple miscarriages.

30-50%
… of early losses occur before a missed period.

40%
… of women with 2+ losses will experience another miscarriage.
Recurrent Pregnancy Loss: A to Z
- What is Recurrent Pregnancy Loss
- The Spectrum of Implantation & Pregnancy Loss
- Embryo Factors
- A Normal Embryo Needs a Normal Uterus
- Synchrony: The Window of Implantation
- Decidualization/Placentation: The Role of NK or “Killer T-cells”
- Decidualization & Placentation: KIR-female/HLAC-male Compatibility
Implantation failure and recurrent pregnancy loss represent a spectrum of problems that result from dyssynchrony between the embryo and endometrium, along with abnormal immune function in the endometrium itself. When early miscarriages are studied carefully, it is clear that almost all the losses occur before 7 weeks. Thus, recurrent IVF “implantation failures”, repeated “chemical pregnancies,” and clinical miscarriages may share some of the same causes.
In the past, patients were subjected to huge blood panels of many antibodies and other immunological markers to decipher treatment. Most of these tests have not been well-studied and are non-specific. Thus, almost all couples were positive for something. Many of the recommended treatments may have been unnecessary, or ineffective. We have developed an approach, in co-operation with one of America’s foremost leaders, the late Dr. Carolyn Coulam, in the evaluation of recurring reproductive failure that is based on sound scientific evidence, and years of combined clinical experience. Our approach is cost effective, not burdensome, and safe.
Implantation failure and pregnancy loss represent a spectrum of problems that share some causes.
Implantation failure can present as longstanding unexplained infertility, or repeated IVF implantation failures with good quality or chromosomally normal embryos. Early pregnancy loss or “biochemical pregnancy” occurs when a woman has a positive pregnancy test, but the pregnancy hormone levels decline before a pregnancy is seen on ultrasound. A clinical miscarriage refers to those losses that occur after a pregnancy is documented by ultrasound. Thus, while all three categories share some causes, we individualize the approach to each patient, based on what type of problem she has experienced. In order for a viable pregnancy to occur, all of the following must be present:
- Normal and viable blastocyst (early embryo)
- Structurally normal uterus
- Synchrony between the endometrium and embryo
- Normal decidualization: changes in the endometrium that permit the embryo to invade into the uterus which are mediated by immunologic processes.
- Placentation: the ability of the embryo vasculature to merge with maternal blood supply and create tiny blood vessels and form a placenta.
Our approach is to evaluate each category and try to understand why a viable pregnancy may not occur, despite conventional treatment.
To learn more about our our Recurrent Pregnancy Loss Program, call us at 866-HRC-4IVF or click the button below:
It is very important to remember that the majority of individual miscarriages are due to abnormal chromosomes in the embryo. This fact clouds the evaluation of recurrent pregnancy loss, because even with repeat miscarriages, abnormal embryos can be the cause. Our evaluation of reproductive failure is strongest when there has been a documented chromosomally normal (euploid) embryo lost at miscarriage or repeat IVF implantation failures with euploid embryos. Even for women who conceive naturally, but experience miscarriages, an IVF attempt with Preimplantation Genetic Testing-for Aneuploidy (PGT-A) may be appropriate to document failure or loss with a euploid embryo.
A rare cause of recurrent pregnancy loss is a chromosomal translocation in either parent. A translocation is when a piece of one chromosome breaks off at conception and sticks to another chromosome. While the person carrying such a rearrangement is healthy because they have all the necessary genetic material, the resulting sperm or eggs have a high chance of having abnormal amounts of DNA. This can result in recurrent miscarriages, and in some cases babies with genetic conditions like Down Syndrome. The incidence of a translocation in the general population is 1/10,000. For couples with three or more miscarriages, the incidence is estimated at 3-5%. So, when a couple has three or more clinical miscarriages, we recommend that both parents have a chromosome analysis (karyotype) to make sure neither one carries a translocation, or other rare conditions.
To learn more about our our Recurrent Pregnancy Loss Program, call us at 866-HRC-4IVF or click the button below:
This is an obvious statement. However, it is surprising how often this simple fact is ignored. We strongly recommend that all women undergoing IVF, especially those with repeat failures, and those with recurrent losses without IVF treatment, have a uterine evaluation. The oldest test available that still gives the most information is the hysterosalpingogram (HSG, or x-ray dye test). An HSG evaluates the uterus and also rules out an abnormality of the fallopian tubes called hydrosalpinx. We can also perform sonohysterogram or hysteroscopy to evaluate the uterine cavity if we are not concerned with the fallopian tubes.
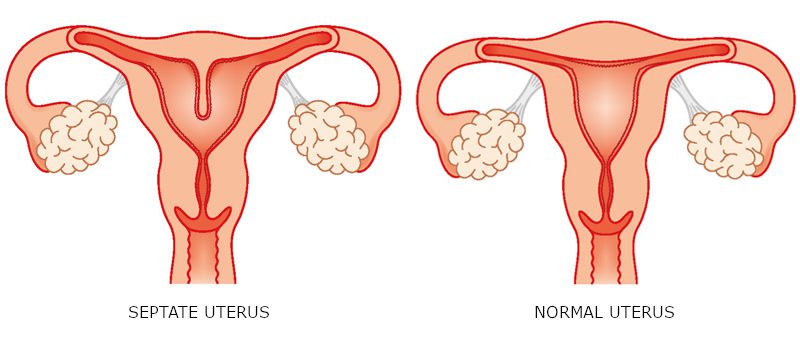
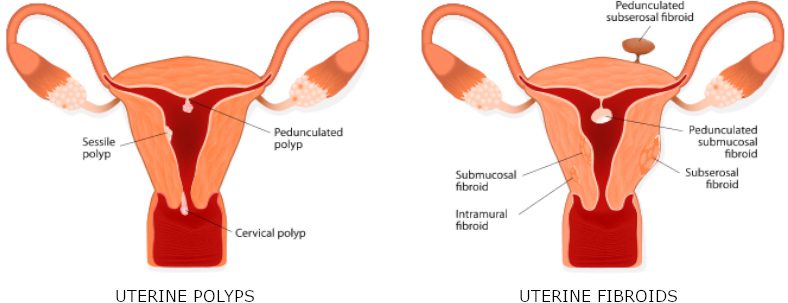
Abnormalities of the cavity that can be seen include uterine septums, scar tissue, polyps and submucous fibroids. Women are born with septums, but can develop the other problems later. A septum is a membrane that divides the uterus into two cavities. Everyone agrees that large septums cause late miscarriages. We have ample experience to show that smaller partial septums can cause IVF failure and even miscarriages. Polyps and submucous fibroids are benign tumors that grow in the uterine cavity and can cause implantation failure. All of these problems can be readily treated with a minor procedure called hysteroscopy.
Another problem that can be found at HSG is hydrosalpinx. A hydrosalpinx is a dilated blocked tube, usually caused by a prior pelvic infection. It has been shown in multiple studies that the presence of a hydrosalpinx reduces IVF success rates by 50%. Although some doctors only recommend removing the tubes if they are large enough to be seen on ultrasound, we generally recommend removal of all such abnormal tubes; especially if there have been failed IVF attempts in the past.
To learn more about our our Recurrent Pregnancy Loss Program, call us at 866-HRC-4IVF or click the button below:
Since the early days of IVF, it has been clear that there is a narrow window of time that the endometrium is receptive to the implantation of a blastocyst. A number of endometrial biopsy tests have been developed to assess this type of uterine receptivity. We use the “Endometrial Receptivity Assay, (ERA),” because it is a good test that can provide guidance for subsequent treatment. The ERA evaluates genetic and molecular markers in the endometrium that have been shown to be critical for normal implantation to occur. The ERA test result will indicate the number of hours of progesterone administration prior to embryo transfer that is needed to a receptive endometrium.
To learn more about our our Recurrent Pregnancy Loss Program, call us at 866-HRC-4IVF or click the button below:
Natural killer (AKA: Killer t-cells) are a type of white blood cells that help destroy foreign bodies like cancer cells and viruses.
In the past, it was assumed that elevated levels of NK cells were detrimental and so blood tests and endometrial biopsy tests were used to detect these cells and offer treatment based on their presence. However, a critical fault of this approach is that there was no consideration for the type of NK cells or whether there was too much or too little of the NK cells.
We offer an endometrial biopsy test that looks for markers on NK cells that help us differentiate the type of NK cells. We can assess whether there are “good” or “bad” NK cells present in the endometrium and whether there is too much or too little that can affect implantation (both decidualization and placentation). In the biopsy we perform we will obtain a decidualization score which tells us the status of the quantity and type of NK cells. Treatment plans are tailored to the result of the decidualization score.
To learn more about our our Recurrent Pregnancy Loss Program, call us at 866-HRC-4IVF or click the button below:
Decidualization and placentation relies on male/female genetic and immunological compatibility. Older testing looked at genetic compatibility, using HLAdq-alpha as the marker. It has become clear that a different HLA marker, HLA C in the male is responsible is responsible for initiating the proper response in the female.
Maternal Natural Killer cells in the endometrium need to be activated in order for decidualization to take place. There are different types of KIR Ligands on the circulating female NK cells. If there is a KIR Ligand with BB or BA antigens, then there is activation to decidualize. However, if the maternal NK cells lack the B type ligand then she would need paternal HLAC to activate the endometrium. If the male has HLAC1 (detected in his blood) then there will be low level activation of the natural killer cells. However, if the female is lacking the activating B ligand and the male partner is also lacking the HLAC1 then there is no activation of the natural killer cells to decidualize. So, if he is HLAC2 (no HLAC1=no male activation) and she does not have the activating B ligand then Neupogen would be beneficial to help the NK cells become more functional.
To learn more about our our Recurrent Pregnancy Loss Program, call us at 866-HRC-4IVF or click the button below:
Comprehensive Work Up & Individualized Treatment Plan
The goal of our Recurrent Pregnancy Loss and Implantation Failure program is to devise a treatment plan that suits each individual patient. Effective treatment depends on the specific etiology. Once we have completed a comprehensive and directed work up, treatment options can include any combination of the following:
- Steroids
- Intralipids
- Endometrial activation by uterine biopsy
- Antibiotics or antivirals
- Blood thinners
- Bone marrow stimulants (Neupogen)
- Immune modulators
- Surgery and alteration of the progesterone regimen
To schedule a consultation with one of our Reproductive Specialists,
call us at 866-HRC-4IVF or click the button below:


